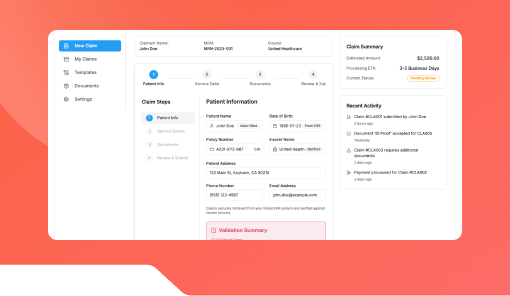
Claim Status Checker Bot
Simplify Health Claim Tracking with AI-Powered Updates
Enable patients and policyholders to instantly check claim progress, approval status, and required documents — all through a conversational AI interface powered by Kriatix.
See Claim Status Checker Bot In Action
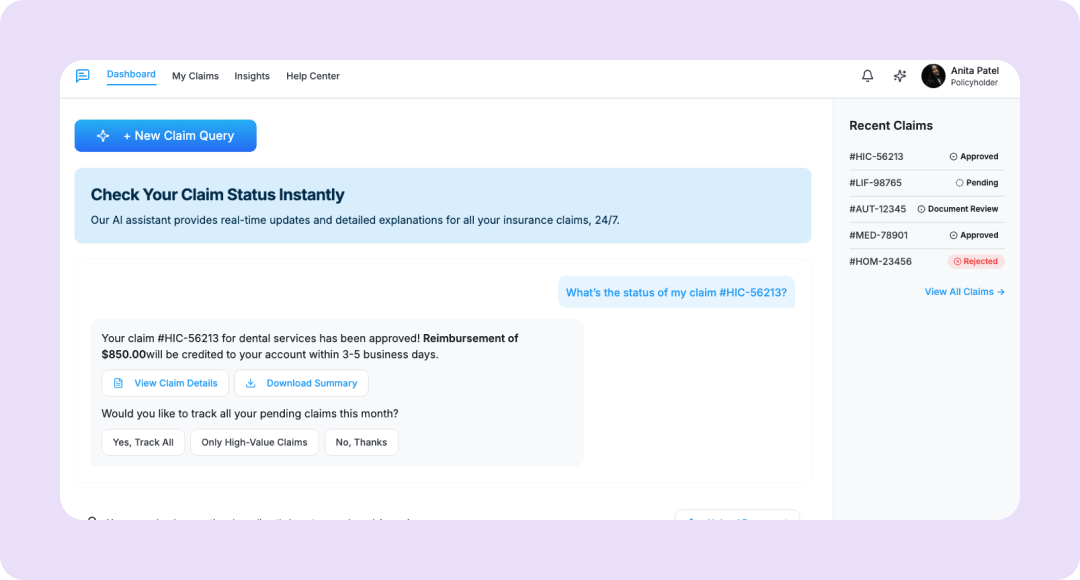
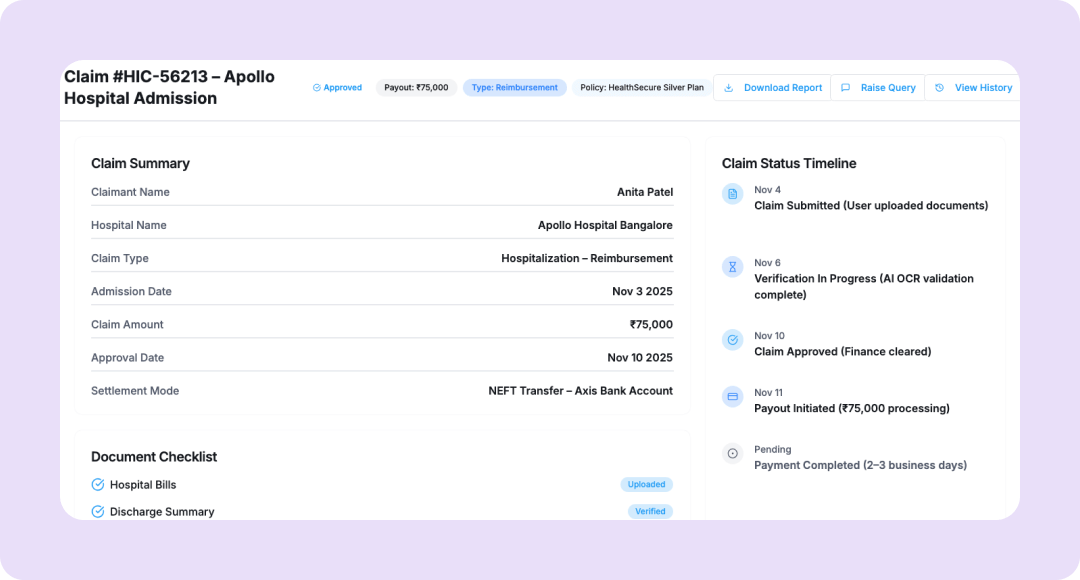
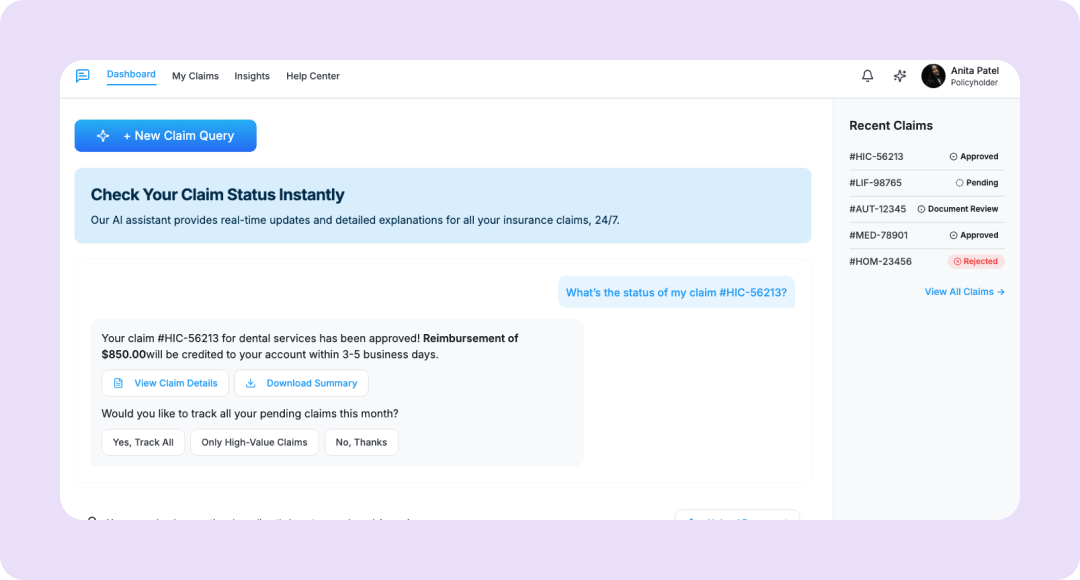
The Claim Status Checker Bot by Kriatix eliminates the frustration of manual insurance claim tracking.
It provides real-time claim updates, document requirements, and estimated timelines directly through chat or web interface. By integrating with insurer APIs and hospital billing systems, it creates a transparent and seamless experience for patients, insurers, and administrators.
🔹 Automate claim status tracking and document verification
🔹 Reduce customer support load for insurers and TPAs
🔹 Deliver 24/7 updates via web, chat, or mobile
What Is the Claim Status Checker Bot?
The Claim Status Checker Bot is a smart conversational assistant designed for healthcare insurers and hospitals. It fetches live claim information from connected insurance or TPA databases, explains current status (submitted, under review, approved, or rejected), and alerts users about pending requirements.
It minimizes manual calls to support centers while ensuring customers receive accurate, real-time updates.
Who Is It For?
| Role | How They Benefit |
|---|---|
| Insurance Providers | Reduce inbound claim status queries |
| Hospitals & TPAs | Improve claim processing transparency |
| Patients/Policyholders | Track claim progress anytime, anywhere |
| Customer Service Teams | Automate repetitive claim inquiries |
| Executives/Compliance Heads | Maintain accuracy and reduce operational delays |
Key Features
- API integration with insurer and TPA claim systems
- Real-time claim status updates and progress visualization
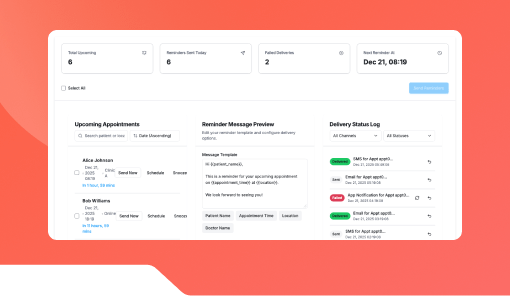
- Notification engine for pending or missing documents
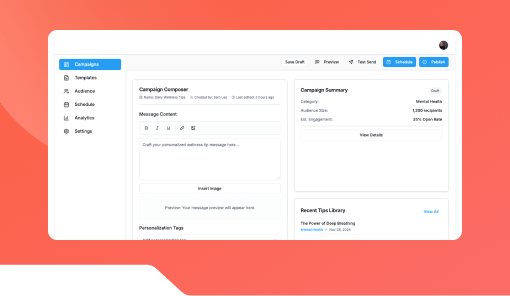
- Multi-channel deployment (web, chat, WhatsApp)
- Policy and claim reference number validation
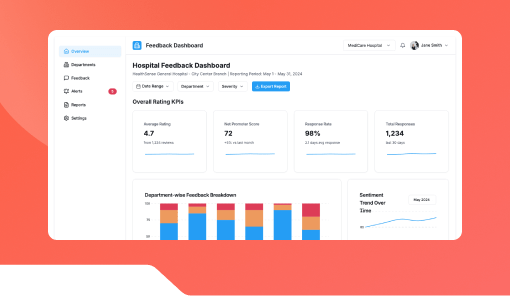
- Analytics dashboard for claim turnaround times
Benefits
- Improve customer experience through proactive updates
- Eliminate long waiting times and manual claim follow-ups
- Reduce claim-related support calls by up to 70%
- Strengthen insurer-patient trust with real-time transparency
- Increase claim handling efficiency through automation
How It Works
- Connect insurer or TPA APIs to the bot engine.
- Patients or policyholders provide claim ID or policy number.
- The bot retrieves claim status and provides detailed updates.
- Sends automated reminders for document submission or verification.
Add-ons & Integrations
- Insurance APIs: MediAssist, Niva Bupa, Star Health, ICICI Lombard
- Messaging Platforms: WhatsApp, Web Chat, Slack, MS Teams
- Hospital Systems: ERP, Billing, and Patient Portals
Deployment & Access
-
- SaaS or on-premise setup
- Web, chat, or in-app interface for patients
- Multi-user dashboard for admin and support teams
What Our Partners Are Saying
Frequently Asked Questions
1. What kind of claim updates can it provide?
It provides status updates such as submitted, under review, approved, settled, or rejected.
2. Does it work for multiple insurers or TPAs?
Yes. It integrates with multiple insurance providers and third-party administrators.
3. How secure is the data?
It uses encrypted channels and follows IRDAI-compliant security protocols.
4. Can it send proactive alerts?
Yes. The system sends alerts for missing documents, upcoming deadlines, or claim settlements.
5. Can it handle multiple claims per user?
Yes. Users can check and track multiple claim IDs within a single conversation.
Ready to Automate Smarter with Kriatix?
Build next-gen, AI-powered apps and workflows—faster, smarter, and tailored to your industry.
Get Started